This is what the CDC has become…
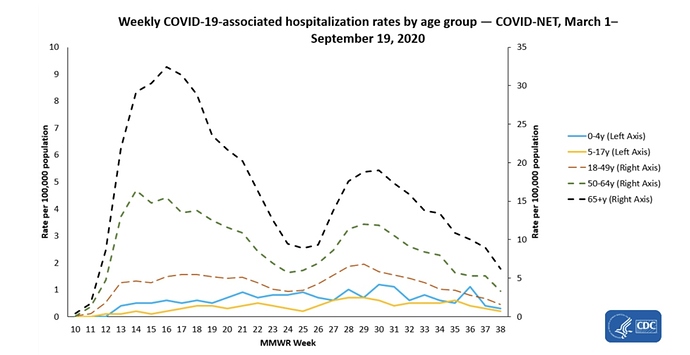
Weekly hospitalization rates among all ages first peaked during the week ending April 18 (MMWR week 16), followed by a second peak during the week ending July 18 (MMWR week 29). From the week ending August 1 (MMWR week 31) to the week ending September 19 (MMWR week 38), weekly hospitalization rates declined for all adult age groups. However, over this same time period, weekly rates remained steady for the pediatric age groups. Data for the most recent weeks may change as additional admissions occurring during those weeks are reported.
Another sign that China is back up on it’s feet before most ever one else.
Copper Rises After Upbeat Chinese Economic Data; China accounts for roughly half of global copper demand, making its manufacturing sector a primary driver of prices
Today 3:14 PM ET Editor’s PicksPrint
By Amrith Ramkumar
Copper prices climbed Wednesday, advancing back toward a multiyear high hit in mid-September after data showed China’s economic recovery is gathering momentum.
Most actively traded copper futures for December delivery added 1.4% to $3.0325 a pound, moving back toward a recent peak of $3.116 hit on Sept. 18.
The industrial metal has risen about 8% for the year and recovered roughly 40% in the past six months following an early-year selloff . Prices tumbled after the Chinese economy shut early during the coronavirus crisis but have benefited with economic activity in the world’s biggest commodity consumer rising lately.
China accounts for roughly half of global copper demand, making its manufacturing sector a primary driver of prices. Copper is a key component of everything from electric vehicles to smartphones.
Figures Wednesday showed China’s official manufacturing purchasing managers index rose more than expected in September , the latest data point indicating an upbeat recovery in China after new coronavirus cases in the country generally stopped rising. A separate private gauge of manufacturing activity also pointed to a healthy rebound driven in part by government stimulus.
The steady pace of economic growth in China during its rebound contrasts with the slowdown some analysts expect to hit the U.S. and Europe, which are grappling with recent rises in coronavirus cases .
Copper’s close ties to China and manufacturing have helped the industrial metal outpace other commodities such as oil that have been hit harder by the pandemic and are more closely linked to global travel.
A Citigroup tool that tracks end uses of copper in China throughout various sectors like appliance makers is also showing robust demand, with the three-month average of the tracker now at its highest level since early in 2017. That highlights “China’s ‘V’ shaped recovery,” Citi analysts said in a note.
Traders will be monitoring economic activity in China during a coming eight-day holiday that begins Thursday. But some analysts also caution that prices for industrial metals could become more volatile because a key source of liquidity will be absent during the coming stretch. Overnight trading during Asian trading hours often sets the tone for the following day’s activity in London and New York.
The US needs to see that our economic future is not dependent on China! We aren’t just fighting a CCP Coronavirus pandemic.
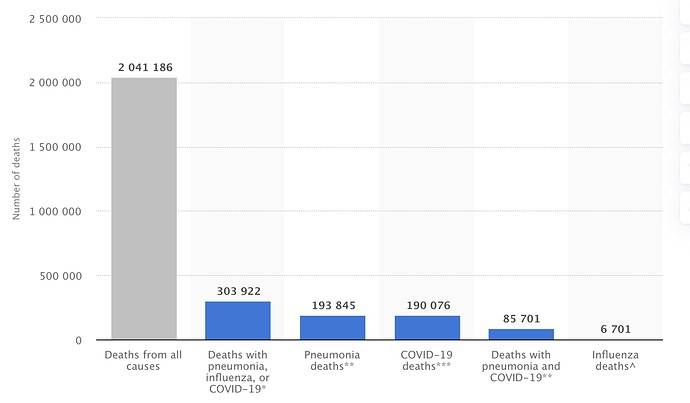
COVID-19, pneumonia, and influenza deaths reported in the U.S. Sep. 19, 2020
Published by John Elflein, Sep 28, 2020
More than 2 million people in the United States died from all causes between the beginning of February and September 19, 2020. Around 190,076 of those deaths were with confirmed or presumed COVID-19. There were also 6,701 fatalities involving influenza, which had pneumonia or COVID-19 also listed as a cause of death.
This next one is a little old, but quite interesting. Wear a mask if you feel you must to prevent spread to the most vulnerable. The citations below this author’s summary conclude masks are not effective. Refutations and update are cited in the link below the author’s original commentary/summary dated August 12. (Yes this is a long cut and paste, both sides of the issue presented. Follow the links.)
Masks Don’t Work: A Review of Science Relevant to COVID-19 Social Policy
By *Denis G. Rancourt, PhD
June 2020Masks and respirators do not work.
There have been extensive randomized controlled trial (RCT) studies, and meta-analysis reviews of RCT studies, which all show that masks and respirators do not work to prevent respiratory influenza-like illnesses, or respiratory illnesses believed to be transmitted by droplets and aerosol particles.
Furthermore, the relevant known physics and biology, which I review, are such that masks and respirators should not work. It would be a paradox if masks and respirators worked, given what we know about viral respiratory diseases: The main transmission path is long-residence-time aerosol particles (< 2.5 μm), which are too fine to be blocked, and the minimum-infective dose is smaller than one aerosol particle.
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
(From Words from the Publisher: “We pledge to publish all letters, guest commentaries, or studies refuting [Rancourt’s] general premise that this mask-wearing culture and shaming could be more harmful than helpful. Please send your feedback to info@rcreader.com.”) [UPDATE: August 12, 2020 Still No Evidence Justifying Mandatory Masks]
Review of the Medical Literature
Here are key anchor points to the extensive scientific literature that establishes that wearing surgical masks and respirators (e.g., “N95”) does not reduce the risk of contracting a verified illness:Jacobs, J. L. et al. (2009) “Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: A randomized controlled trial,” American Journal of Infection Control , Volume 37, Issue 5, 417 – 419. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial - PubMed
N95-masked health-care workers (HCW) were significantly more likely to experience headaches. Face mask use in HCW was not demonstrated to provide benefit in terms of cold symptoms or getting colds.
Cowling, B. et al. (2010) “Face masks to prevent transmission of influenza virus: A systematic review,” Epidemiology and Infection , 138(4), 449-456. https://www.cambridge.org/core/journals/epidemiology-and-infection/article/face-masks-to-prevent-transmission-of-influenza-virus-a-systematic- review/64D368496EBDE0AFCC6639CCC9D8BC05
None of the studies reviewed showed a benefit from wearing a mask, in either HCW or community members in households (H). See summary Tables 1 and 2 therein.
bin-Reza et al. (2012) “The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence,” Influenza and Other Respiratory Viruses 6(4), 257–267. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1750-2659.2011.00307.x
“There were 17 eligible studies. … None of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.”
Smith, J.D. et al. (2016) “Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis,” CMAJ Mar 2016 https://www.cmaj.ca/content/188/8/567
“We identified six clinical studies … . In the meta-analysis of the clinical studies, we found no significant difference between N95 respirators and surgical masks in associated risk of (a) laboratory-confirmed respiratory infection, (b) influenza-like illness, or (c) reported work-place absenteeism.”
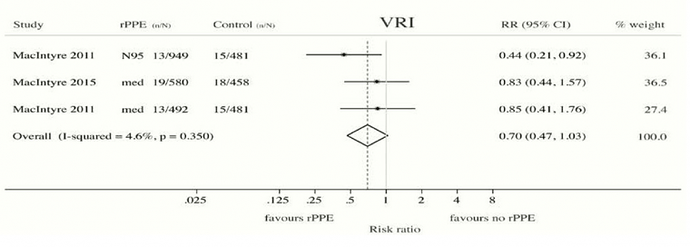
Offeddu, V. et al. (2017) “Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis,” Clinical Infectious Diseases , Volume 65, Issue 11, 1 December 2017, Pages 1934–1942, https://academic.oup.com/cid/article/65/11/1934/4068747
“Self-reported assessment of clinical outcomes was prone to bias. Evidence of a protective effect of masks or respirators against verified respiratory infection (VRI) was not statistically significant”; as per Fig. 2c therein:
Radonovich, L.J. et al. (2019) “N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial,” JAMA . 2019; 322(9): 824–833. N95 Respirators vs Medical Masks for Preventing Laboratory-Confirmed Influenza in Health Care Personnel
“Among 2862 randomized participants, 2371 completed the study and accounted for 5180 HCW-seasons. … Among outpatient health care personnel, N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza.”
Long, Y. et al. (2020) “Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis,” J Evid Based Med. 2020; 1- 9. https://onlinelibrary.wiley.com/doi/epdf/10.1111/jebm.12381
“A total of six RCTs involving 9,171 participants were included. There were no statistically significant differences in preventing laboratory-confirmed influenza, laboratory-confirmed respiratory viral infections, laboratory-confirmed respiratory infection, and influenza-like illness using N95 respirators and surgical masks. Meta-analysis indicated a protective effect of N95 respirators against laboratory-confirmed bacterial colonization (RR = 0.58, 95% CI 0.43-0.78). The use of N95 respirators compared with surgical masks is not associated with a lower risk of laboratory-confirmed influenza.”
Conclusion Regarding That Masks Do Not Work
No RCT study with verified outcome shows a benefit for HCW or community members in households to wearing a mask or respirator. There is no such study. There are no exceptions.Likewise, no study exists that shows a benefit from a broad policy to wear masks in public (more on this below).
Furthermore, if there were any benefit to wearing a mask, because of the blocking power against droplets and aerosol particles, then there should be more benefit from wearing a respirator (N95) compared to a surgical mask, yet several large meta-analyses, and all the RCT, prove that there is no such relative benefit.
Masks and respirators do not work.
Precautionary Principle Turned on Its Head with Masks
In light of the medical research, therefore, it is difficult to understand why public-health authorities are not consistently adamant about this established scientific result, since the distributed psychological, economic, and environmental harm from a broad recommendation to wear masks is significant, not to mention the unknown potential harm from concentration and distribution of pathogens on and from used masks. In this case, public authorities would be turning the precautionary principle on its head (see below).Physics and Biology of Viral Respiratory Disease and of Why Masks Do Not Work
In order to understand why masks cannot possibly work, we must review established knowledge about viral respiratory diseases, the mechanism of seasonal variation of excess deaths from pneumonia and influenza, the aerosol mechanism of infectious disease transmission, the physics and chemistry of aerosols, and the mechanism of the so-called minimum-infective-dose.In addition to pandemics that can occur anytime, in the temperate latitudes there is an extra burden of respiratory-disease mortality that is seasonal, and that is caused by viruses. For example, see the review of influenza by Paules and Subbarao (2017). This has been known for a long time, and the seasonal pattern is exceedingly regular. (Publisher’s note: All links to source references to studies here forward are found at the end of this article.)
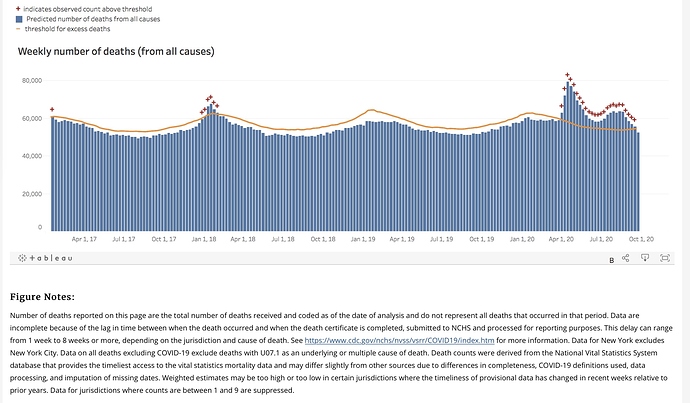
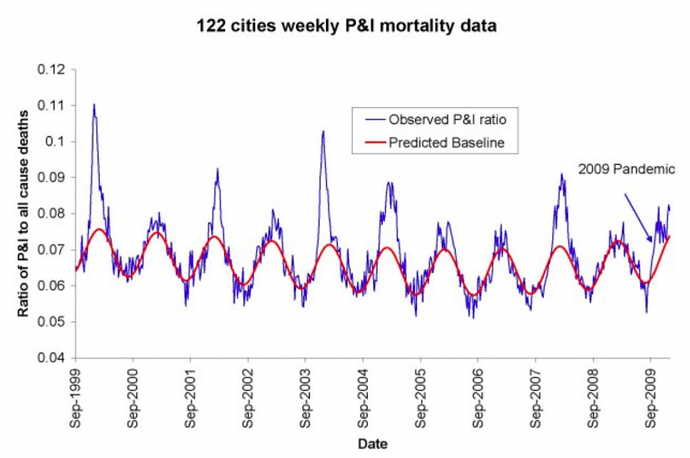
For example, see Figure 1 of Viboud (2010), which has “Weekly time series of the ratio of deaths from pneumonia and influenza to all deaths, based on the 122 cities surveillance in the US (blue line). The red line represents the expected baseline ratio in the absence of influenza activity,” here:
The seasonality of the phenomenon was largely not understood until a decade ago. Until recently, it was debated whether the pattern arose primarily because of seasonal change in virulence of the pathogens, or because of seasonal change in susceptibility of the host (such as from dry air causing tissue irritation, or diminished daylight causing vitamin deficiency or hormonal stress). For example, see Dowell (2001).
In a landmark study, Shaman et al. (2010) showed that the seasonal pattern of extra respiratory-disease mortality can be explained quantitatively on the sole basis of absolute humidity, and its direct controlling impact on transmission of airborne pathogens.
Lowen et al. (2007) demonstrated the phenomenon of humidity-dependent airborne-virus virulence in actual disease transmission between guinea pigs, and discussed potential underlying mechanisms for the measured controlling effect of humidity.
The underlying mechanism is that the pathogen-laden aerosol particles or droplets are neutralized within a half-life that monotonically and significantly decreases with increasing ambient humidity. This is based on the seminal work of Harper (1961). Harper experimentally showed that viral-pathogen-carrying droplets were inactivated within shorter and shorter times, as ambient humidity was increased.
Harper argued that the viruses themselves were made inoperative by the humidity (“viable decay”), however, he admitted that the effect could be from humidity-enhanced physical removal or sedimentation of the droplets (“physical loss”): “Aerosol viabilities reported in this paper are based on the ratio of virus titre to radioactive count in suspension and cloud samples, and can be criticized on the ground that test and tracer materials were not physically identical.”
The latter (“physical loss”) seems more plausible to me, since humidity would have a universal physical effect of causing particle/droplet growth and sedimentation, and all tested viral pathogens have essentially the same humidity-driven “decay.” Furthermore, it is difficult to understand how a virion (of all virus types) in a droplet would be molecularly or structurally attacked or damaged by an increase in ambient humidity. A “virion” is the complete, infective form of a virus outside a host cell, with a core of RNA or DNA and a capsid. The actual mechanism of such humidity-driven intra-droplet “viable decay” of a virion has not been explained or studied.
In any case, the explanation and model of Shaman et al. (2010) is not dependent on the particular mechanism of the humidity-driven decay of virions in aerosol/droplets. Shaman’s quantitatively demonstrated model of seasonal regional viral epidemiology is valid for either mechanism (or combination of mechanisms), whether “viable decay” or “physical loss.”
The breakthrough achieved by Shaman et al. is not merely some academic point. Rather, it has profound health-policy implications, which have been entirely ignored or overlooked in the current coronavirus pandemic.
In particular, Shaman’s work necessarily implies that, rather than being a fixed number (dependent solely on the spatial-temporal structure of social interactions in a completely susceptible population, and on the viral strain), the epidemic’s basic reproduction number (R0) is highly or predominantly dependent on ambient absolute humidity.
For a definition of R0, see HealthKnowlege-UK (2020): R0 is “the average number of secondary infections produced by a typical case of an infection in a population where everyone is susceptible.” The average R0 for influenza is said to be 1.28 (1.19–1.37); see the comprehensive review by Biggerstaff et al. (2014).
In fact, Shaman et al. showed that R0 must be understood to seasonally vary between humid-summer values of just larger than “1” and dry-winter values typically as large as “4” (for example, see their Table 2). In other words, the seasonal infectious viral respiratory diseases that plague temperate latitudes every year go from being intrinsically mildly contagious to virulently contagious, due simply to the bio-physical mode of transmission controlled by atmospheric humidity, irrespective of any other consideration.
Therefore, all the epidemiological mathematical modeling of the benefits of mediating policies (such as social distancing), which assumes humidity-independent R0 values, has a large likelihood of being of little value, on this basis alone. For studies about modeling and regarding mediation effects on the effective reproduction number, see Coburn (2009) and Tracht (2010).
To put it simply, the “second wave” of an epidemic is not a consequence of human sin regarding mask wearing and hand shaking. Rather, the “second wave” is an inescapable consequence of an air-dryness-driven many-fold increase in disease contagiousness, in a population that has not yet attained immunity.
If my view of the mechanism is correct (i.e., “physical loss”), then Shaman’s work further necessarily implies that the dryness-driven high transmissibility (large R0) arises from small aerosol particles fluidly suspended in the air; as opposed to large droplets that are quickly gravitationally removed from the air.
Such small aerosol particles fluidly suspended in air, of biological origin, are of every variety and are everywhere, including down to virion-sizes (Despres, 2012). It is not entirely unlikely that viruses can thereby be physically transported over inter-continental distances (e.g., Hammond, 1989).
More to the point, indoor airborne virus concentrations have been shown to exist (in day-care facilities, health centers, and on-board airplanes) primarily as aerosol particles of diameters smaller than 2.5 μm, such as in the work of Yang et al. (2011):
“Half of the 16 samples were positive, and their total virus −3 concentrations ranged from 5800 to 37 000 genome copies m . On average, 64 per cent of the viral genome copies were associated with fine particles smaller than 2.5 μm, which can remain suspended for hours. Modeling of virus concentrations indoors suggested a source strength of 1.6 ± 1.2 × 105 genome copies m−3 air h−1 and a deposition flux onto surfaces of 13 ± 7 genome copies m−2 h−1 by Brownian motion. Over one hour, the inhalation dose was estimated to be 30 ± 18 median tissue culture infectious dose (TCID50), adequate to induce infection. These results provide quantitative support for the idea that the aerosol route could be an important mode of influenza transmission.”
Such small particles (< 2.5 μm) are part of air fluidity, are not subject to gravitational sedimentation, and would not be stopped by long-range inertial impact. This means that the slightest (even momentary) facial misfit of a mask or respirator renders the design filtration norm of the mask or respirator entirely irrelevant. In any case, the filtration material itself of N95 (average pore size ~0.3−0.5 μm) does not block virion penetration, not to mention surgical masks. For example, see Balazy et al. (2006).
Mask stoppage efficiency and host inhalation are only half of the equation, however, because the minimal infective dose (MID) must also be considered. For example, if a large number of pathogen-laden particles must be delivered to the lung within a certain time for the illness to take hold, then partial blocking by any mask or cloth can be enough to make a significant difference.
On the other hand, if the MID is amply surpassed by the virions carried in a single aerosol particle able to evade mask-capture, then the mask is of no practical utility, which is the case.
Yezli and Otter (2011), in their review of the MID, point out relevant features:
- Most respiratory viruses are as infective in humans as in tissue culture having optimal laboratory susceptibility
- It is believed that a single virion can be enough to induce illness in the host
- The 50-percent probability MID (“TCID50”) has variably been found to be in the range 100−1000 virions
- There are typically 10 to 3rd power − 10 to 7th power virions per aerolized influenza droplet with diameter 1 μm − 10 μm
- The 50-percent probability MID easily fits into a single (one) aerolized droplet
- For further background:
- A classic description of dose-response assessment is provided by Haas (1993).
- Zwart et al. (2009) provided the first laboratory proof, in a virus-insect system, that the action of a single virion can be sufficient to cause disease.
- Baccam et al. (2006) calculated from empirical data that, with influenza A in humans,“we estimate that after a delay of ~6 h, infected cells begin producing influenza virus and continue to do so for ~5 h. The average lifetime of infected cells is ~11 h, and the half-life of free infectious virus is ~3 h. We calculated the [in-body] basic reproductive number, R0, which indicated that a single infected cell could produce ~22 new productive infections.”
- Brooke et al. (2013) showed that, contrary to prior modeling assumptions, although not all influenza-A-infected cells in the human body produce infectious progeny (virions), nonetheless, 90 percent of infected cell are significantly impacted, rather than simply surviving unharmed.
All of this to say that: if anything gets through (and it always does, irrespective of the mask), then you are going to be infected. Masks cannot possibly work. It is not surprising, therefore, that no bias-free study has ever found a benefit from wearing a mask or respirator in this application.
Therefore, the studies that show partial stopping power of masks, or that show that masks can capture many large droplets produced by a sneezing or coughing mask-wearer, in light of the above-described features of the problem, are irrelevant. For example, such studies as these: Leung (2020), Davies (2013), Lai (2012), and Sande (2008).
Why There Can Never Be an Empirical Test of a Nation-Wide Mask-Wearing Policy
As mentioned above, no study exists that shows a benefit from a broad policy to wear masks in public. There is good reason for this. It would be impossible to obtain unambiguous and bias-free results [because]:
- Any benefit from mask-wearing would have to be a small effect, since undetected in controlled experiments, which would be swamped by the larger effects, notably the large effect from changing atmospheric humidity.
- Mask compliance and mask adjustment habits would be unknown.
- Mask-wearing is associated (correlated) with several other health behaviors; see Wada (2012).
- The results would not be transferable, because of differing cultural habits.
- Compliance is achieved by fear, and individuals can habituate to fear-based propaganda, and can have disparate basic responses.
- Monitoring and compliance measurement are near-impossible, and subject to large errors.
- Self-reporting (such as in surveys) is notoriously biased, because individuals have the self-interested belief that their efforts are useful.
- Progression of the epidemic is not verified with reliable tests on large population samples, and generally relies on non-representative hospital visits or admissions.
- Several different pathogens (viruses and strains of viruses) causing respiratory illness generally act together, in the same population and/or in individuals, and are not resolved, while having different epidemiological characteristics.
Unknown Aspects of Mask Wearing
Many potential harms may arise from broad public policies to wear masks, and the following unanswered questions arise:
- Do used and loaded masks become sources of enhanced transmission, for the wearer and others?
- Do masks become collectors and retainers of pathogens that the mask wearer would otherwise avoid when breathing without a mask?
- Are large droplets captured by a mask atomized or aerolized into breathable components? Can virions escape an evaporating droplet stuck to a mask fiber?
- What are the dangers of bacterial growth on a used and loaded mask?
- How do pathogen-laden droplets interact with environmental dust and aerosols captured on the mask?
- What are long-term health effects on HCW, such as headaches, arising from impeded breathing?
- Are there negative social consequences to a masked society?
- Are there negative psychological consequences to wearing a mask, as a fear-based behavioral modification?
- What are the environmental consequences of mask manufacturing and disposal?
- Do the masks shed fibers or substances that are harmful when inhaled?
Conclusion
By making mask-wearing recommendations and policies for the general public, or by expressly condoning the practice, governments have both ignored the scientific evidence and done the opposite of following the precautionary principle.In an absence of knowledge, governments should not make policies that have a hypothetical potential to cause harm. The government has an onus barrier before it instigates a broad social-engineering intervention, or allows corporations to exploit fear-based sentiments.
Furthermore, individuals should know that there is no known benefit arising from wearing a mask in a viral respiratory illness epidemic, and that scientific studies have shown that any benefit must be residually small, compared to other and determinative factors.
Otherwise, what is the point of publicly funded science?
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
Denis G. Rancourt is a researcher at the Ontario Civil Liberties Association (OCLA.ca) and is formerly a tenured professor at the University of Ottawa, Canada. This paper was originally published at Rancourt’s account on ResearchGate.net. As of June 5, 2020, this paper was removed from his profile by its administrators at Rese archgate.net/profile/D_Rancourt . At Rancourt’s blog ActivistTeacher . blogspot.com, he recounts the notification and responses he received from ResearchGate.net and states, “This is censorship of my scientific work like I have never experienced before.”
The original April 2020 white paper in .pdf format is available here, complete with charts that have not been reprinted in the Reader print or web versions.
RELATED COMMENTARY: An Unprecedented Experiment: Sometimes You Just Gotta Wear the Stupid
Blockquote
172 studies reviewed. Conclusion…wear a mask!
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31142-9/fulltext#%20
As previously stated, the scientific debate about the usefulness of masks in slowing the spread and decreasing the severity of Covid is over. It remains a topic of discussion only in political circles.
Some positive news; social distancing and mask wearing world wide has nearly eliminated the flu! Currently, there is only one outbreak detected which happens to be in Cambodia! Even there, the particular flu strain is a mild one.
“A closed mind is a terrible thing to waste.” Who said that!
Pay attention to who and what is being censored and why.
Denis G. Rancourt used extensive randomized controlled trial studies and meta-analysis reviews in citations from many professional publications. He had an important point of view to convey.
Is the data really unequivocal? After reviewing it I don’t think it is.
The study commentary says, “No randomised trials were identified for these interventions in COVID-19, SARS, or MERS.” Are randomized studies the “gold standard” to use before accepting validity?
“172 observational studies across 16 countries and six continents, with no randomised controlled trials”
I think face masks are appropriate in some settings, but make no sense whatsoever in other settings. Can’t we start using common sense?
Have you heard of the “Publish or Perish” aphorism describing the pressure in academic circles to publish? It is very competitive. It is interesting to note how extensive the Lancet study was with contributions by many authors and institutions. I’m sure it was costly as well as timely, but it was specifically stated to be used as interim guidance for policy makers. This Lancet systematic review was commissioned and in part paid for by WHO! I guess we shouldn’t comment on the funding.
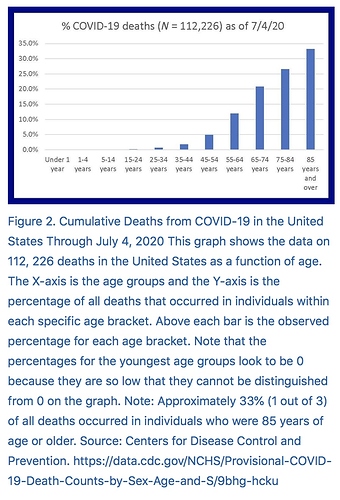
Undoubtedly Covid-19 is a very transmissible disease, greater than most corona viruses. The most vulnerable groups have been identified and need all extra precautions taken to protect them from contracting the disease; But what groups are least affected by the most severe consequences of the infection? Is the spread controllable? It appears from the bulk of all information available that distance, and sanitation have the greatest effect in controlling the disease. Other factors are length of time of the exposure, and size of the exposure. It is also surmised by virologists that normal human immune responses may build up immunity to many diseases when small exposures are encountered to infectious diseases. Repeated small exposures may actually build up a level of antibodies that render the individual immune to the disease over time. The titer level offering immunity for Covid-19 has not yet been quantified. Also the full role of T cells is still being studied. It is best to keep an open mind to all points of view in overcoming the most deleterious effect of the Covid-19 coronavirus.Those under 24 have an associated mortality of <0.1%.
I do disagree with your conclusion concerning mask usage “in slowing the spread and decreasing the severity of Covid is over.” I agree the same social distancing and sanitation measures that are used to fight Covid-19 are very effective in eliminating the flu to a large degree. Masks are commonly used around those bedridden with the flu, but people don’t usually wear a mask all day while at work during flu season. Maybe we will this year. Further, “the cure” cannot be allowed to be worse than the socio-economic effects of the disease itself. Mandatory use of masks in all circumstances is unwarranted and should not be used to distance people or discussions on best practices. We are aware of the factors needed to protect the most vulnerable within the population. We do not need to destroy our livelihoods and economy to meet the political ends of one political party or another. Practicing safe distancing and hygienic measures are practical and just common sense. It is time to stop using some science while completely ignoring other science.
I see in the news this morning that the most prominent anti masker of them all has the virus! 
Positive HCQ Treatment Outcomes in 88 International Studies
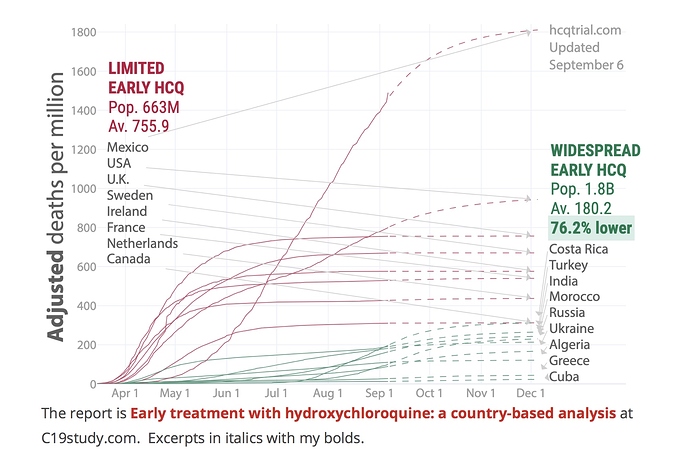
Many countries either adopted or declined early treatment with HCQ, effectively forming a large trial with 1.8 billion people in the treatment group and 663 million in the control group . As of September 6, 2020, an average of 57.4 per million in the treatment group have died, and 466.4 per million in the control group, relative risk 0.123. After adjustments, treatment and control deaths become 119.6 per million and 694.7 per million, relative risk 0.17. The probability of an equal or lower relative risk occurring from random group assignments is 0.008. Accounting for predicted changes in spread, we estimate a relative risk of 0.24. The treatment group has a 76.2% lower death rate . Confounding factors affect this estimate. We examined diabetes, obesity, hypertension, life expectancy, population density, urbanization, testing level, and intervention level, which do not account for the effect observed.
The treatment group countries generally show significantly slower growth in mortality which may be due to treatment, interventions, differences in culture, or the initial degree of infections arriving into the country. Over time we expect that increasingly similar percentages of people will have been exposed , since it is unlikely that the virus will be eliminated soon.
Positive HCQ Treatment Outcomes in 88 International Studies | Science Matters
So, what has changed? Two totally different perspectives of what we see happening and the news that is reported. Science is based on facts, not just opinions. Far too many opinions that are more than just biased, but news is news?
White House coronavirus adviser Scott Atlas reacts to Trump’s coronavirus diagnosis, says ‘zero reason to panic’
“It is no surprise that people get the infection, even with precautions,” Atlas said. “I anticipate a complete and full and rapid recovery back to normal after his necessary confinement period. I anticipate he’ll be back on the road and in full swing.”
… “This is a widespread, highly contagious infection, and this is going to be very mild or asymptomatic for the overwhelming majority of people, especially if you’re a healthy person,” he explained. “And if you can, do your best at the usual mitigation — hand washing, social distancing, the usual masks, if you are in very tight spaces and you cannot socially distance, or are with high-risk family members.”
He added: “This is a disease that spreads, we anticipate that people get this infection, and it does not go away by isolating or locking down.”
“There is zero reason to panic,” Atlas said. “There is nothing different here. The president and his wife are human beings.”
Atlas stressed that the president “always” takes precautions, following social distancing guidelines, and said he is tested regularly, and “wears a mask in appropriate settings.”
“We know the severe harms of locking down with prolonged isolation and prolonged closures of schools and businesses, and nothing has changed about the message—which is, this is a widespread infection, the vast majority of people do well, we need to protect the highest risk people and open schools up and society and get back to functioning,” Atlas said.
He added: “We are all highly optimistic at the White House.”
Here’s the other version of Dr. Scott Atlas’s remarks.
A New Coronavirus Adviser Roils the White House With Unorthodox Ideas
Dr. Scott Atlas arrived at the White House as a coronavirus contrarian, questioning controls like masks. He has angered top health officials while pushing a suite of disputed policy prescriptions.
https://www.nytimes.com/2020/09/02/us/politics/trump-scott-atlas-coronavirus.html
Both of these news reports are biased with a basis in facts. I like hearing both sides!
Too bad all of your treasonous leaders are getting the Covid, and NOT wearing masks. Go figure!
Your decision to follow the uneducated “scientists” down the death hole is fine, but please stop regurgitating their (and your) asinine conclusions.
Right-wing conspiracies should stay in the trash bin where they came from…
I see credible reports that Trump is already having trouble breathing and hence the sudden airlift to the hospital. Based on his disease progression and risk profile, he has a 85 to 90 percent chance of survival at this point. I think it very likely that he will remain in pretty crappy shape most of October. Pence and maybe even Biden are now at risk for testing positive in the next couple of days.
“uneducated “scientists”” - now that’s funny - and a fool’s statement
Based on what? I’ve seen survival for the President quoted at 99.4%! Since there is no credible source for either, we both could say most anything here. It’s all just opinion. That’s why I do like to show sources that have some validity, along with personal commentary. The statistic for mortality I’ve started to see lately for those under age 40 from SARS-CoV-2 is 0.2% and for most seasonal flu around 0.1%. Is the lower mortality for seasonal flu attributed to vaccine use? This makes a very strong case for those who are able to return to work with appropriate precautions in the workplace and home to do so. I’ve also heard that in NY city only 10% of office workers have returned to “the office”. This is completely devastating much more than real estate, not to mention all the restaurants that depended on their business from these daily commuters. The high end restaurants around the UN are out of business, and the airline travel is devastated. The impact of some policies will completely devastate some cities and states unnecessarily. The purpose of early shutdown policies was not to eliminate all risk of spread of the virus.
Deaths should be minimized but need to be reasonably balanced with survivability of cities and states and country. The contagion has spread to far more than reported, many more than just those being tested, yet hospitalizations and death rates continue to drop.
Interesting to think there may be evidence pointing to the cause of high transmission of the virus.
Pain relief caused by SARS-CoV-2 infection may help explain COVID-19 spread
by Stacy Pigott, University of Arizona Oct 1
“It made a lot of sense to me that perhaps the reason for the unrelenting spread of COVID-19 is that in the early stages, you’re walking around all fine as if nothing is wrong because your pain has been suppressed,” said Dr. Khanna. “You have the virus, but you don’t feel bad because you pain is gone. If we can prove that this pain relief is what is causing COVID-19 to spread further, that’s of enormous value.”The paper, “SARS-CoV-2 Spike protein co-opts VEGF-A/Neuropilin-1 receptor signalingto induce analgesia,” will be published in PAIN , the journal of the International Association for the Study of Pain.
The U.S. Centers for Disease Control and Prevention released updated data Sept. 10 estimating 50% of COVID-19 transmission occurs prior to the onset of symptoms and 40% of COVID-19 infections are asymptomatic.
Pain relief caused by SARS-CoV-2 infection may help explain COVID-19 spread
Very true!
You can fool all the people some of the time , and some of the people all the time , but you cannot fool all the people all the time .- Abraham Lincoln
Easy, you have lost all credibility with me. Please dont bother to reply to my posts. Thanks.
Just ignore anything I post then. If I disagree with some of your opinions I will voice my opinion and substantiate them based on credible sources and information. My comments and point of view are my own. Science is science and scientists frequently disagree.
A closed mind is a terrible thing to waste. Catastrophic examples can be found throughout history. If a person stops learning there is no growth and no progress. Think about it!
Trump survived the first wave of the virus with 103 F fever, low blood oxygen levels and heart palpitations. Trump has improved but risks further down turns as typically the virus waxes and wanes a number of times until one recovers. Perhaps the experimental antibody cocktail he is on is working so he is already recovering?
Dave, 35 years in the fire service with no politics on masks.I taught the state hazardous materials technician class to hundreds of firefighters across the state. NIOH standards dictated ppe down to the parts per million(ppm) I have been in every environment you can imagine. I was on a fire truck for AIDS, MERS. you are wrong and the president is wrong, easymillion is endangering lives.
Kevin (and Easy),
You just don’t get my comment. It was just about the “uneducated “scientists” wording. Are there really any or was that just an uneducated comment?
My comment has nothing to do with politics or political party. Shame on you for assuming that.
Rumor that VP Pence has COVID. This appears to be based on two things. He had “pink eye” at the debate which can be a symptom of COVID and also he suddenly canceled plans in AZ without explanation and is now flying back to Wash